Chapter 3
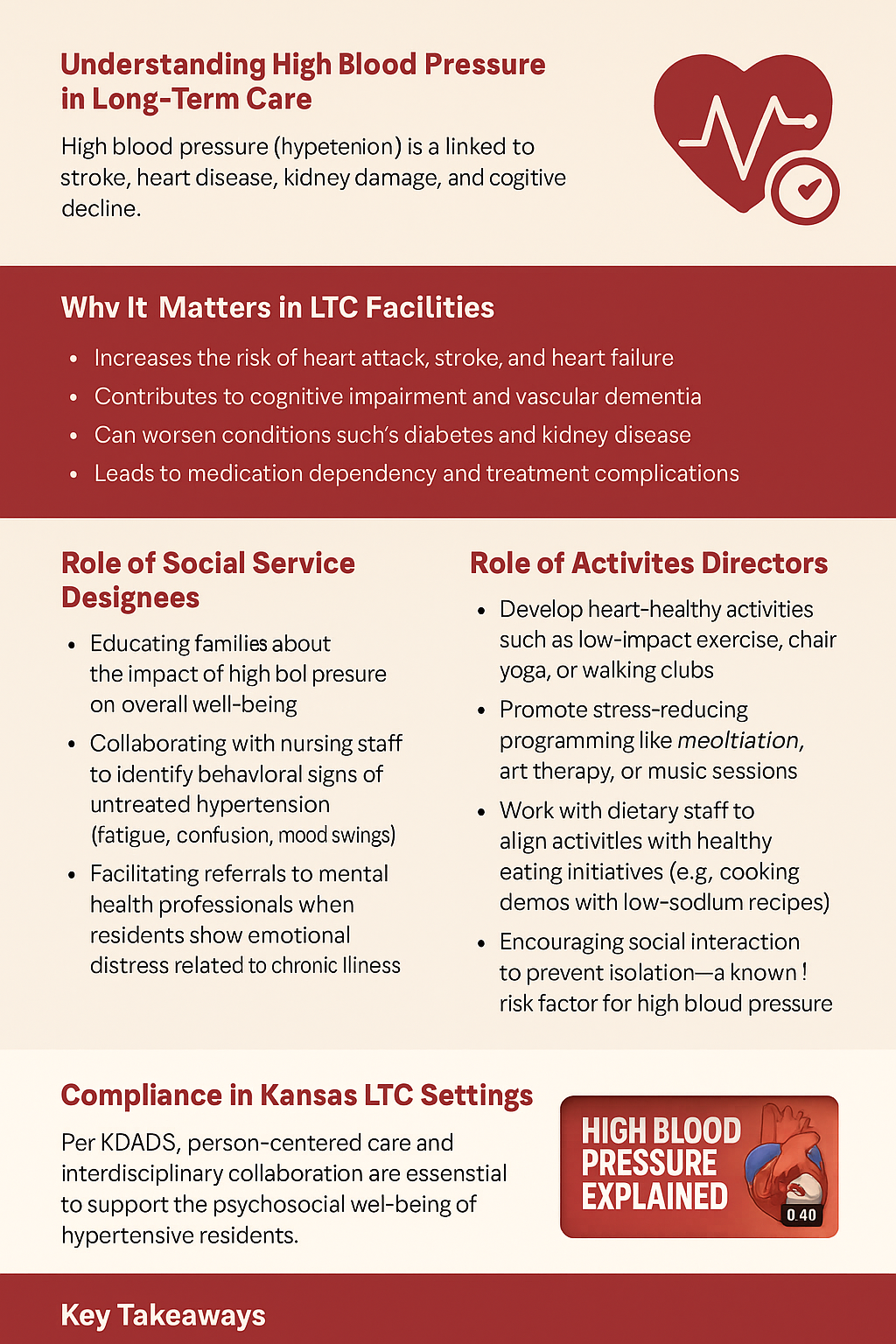
High blood pressure (hypertension) is a chronic condition affecting millions of older adults. In long-term care (LTC) settings, managing hypertension is critical due to its links to stroke, heart disease, kidney damage, and cognitive decline. As Social Service Designees (SSDs) and Activity Directors (ADs), understanding the social, emotional, and physical impact of high blood pressure allows you to better support residents' needs and help coordinate holistic care.
High blood pressure occurs when the force of the blood pushing against artery walls is consistently too high. Normal readings are below 120/80 mmHg. Persistent readings above 130/80 mmHg are considered elevated or hypertensive. This condition often presents no symptoms, which is why it's called the “silent killer.”
SSDs help residents and families cope with the emotional and social challenges of chronic diseases like hypertension. Responsibilities include:
Physical activity and mental engagement are powerful tools in hypertension management. ADs can:
According to Kansas Department for Aging and Disability Services (KDADS), person-centered care and interdisciplinary collaboration are essential. SSDs and ADs must work as part of the care team to support the psychosocial well-being of hypertensive residents, ensuring plans of care meet both medical and quality-of-life goals.
Sources:
Centers for Disease Control and Prevention (CDC). "High Blood Pressure." Retrieved from https://www.cdc.gov/bloodpressure/
Kansas Department for Aging and Disability Services (KDADS). LTC Policies and Resources. https://www.kdads.ks.gov