Chapter 3
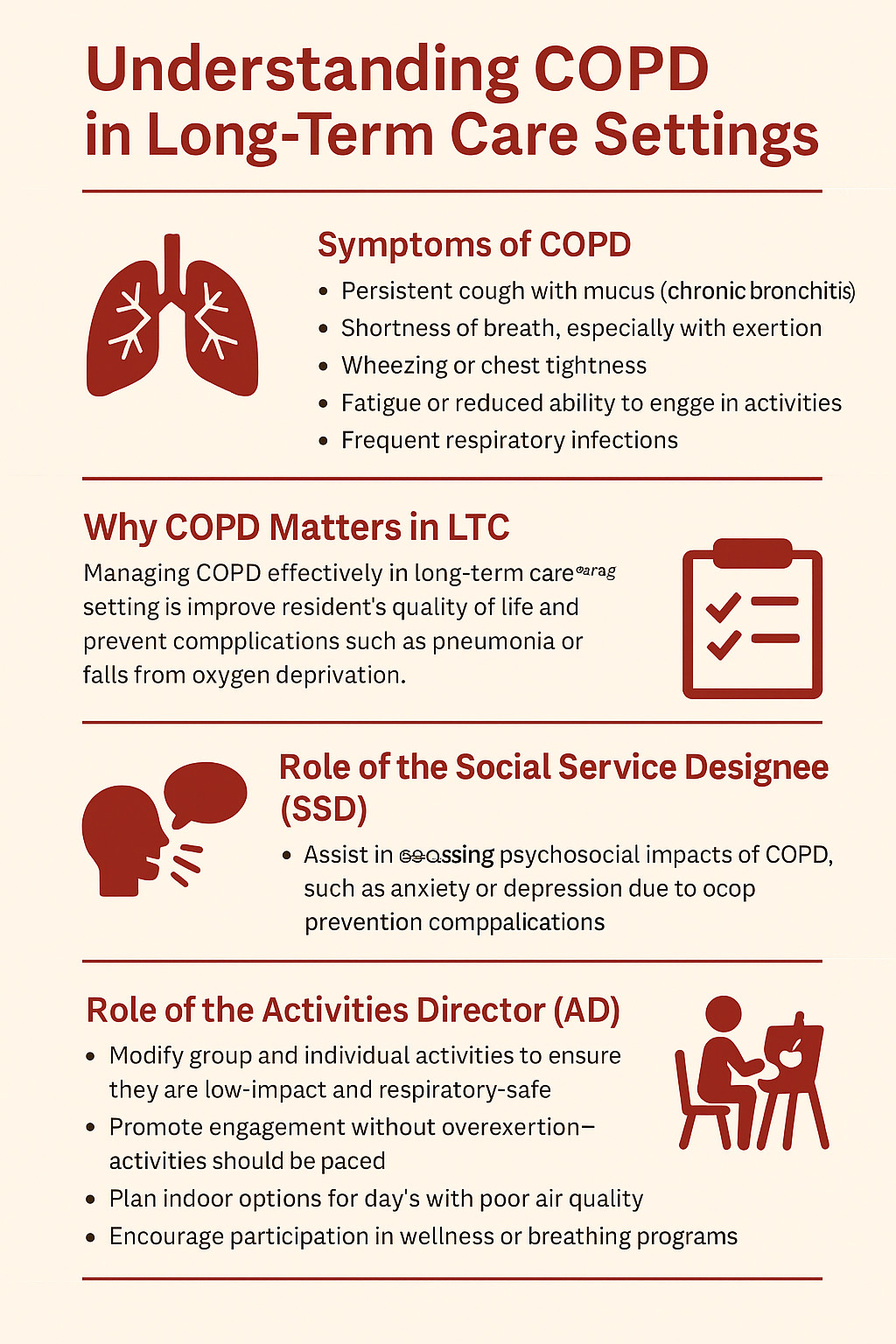
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung condition that includes chronic bronchitis and emphysema. It limits airflow and makes breathing difficult. COPD is common among elderly residents in long-term care (LTC) facilities, especially those with a history of smoking or prolonged exposure to lung irritants.
Managing COPD effectively in a long-term care setting is crucial to improving the resident's quality of life and preventing complications such as pneumonia, falls from oxygen deprivation, or hospitalization. This is especially important in Kansas, where regulations emphasize resident-centered care and maintaining functional abilities.
Under Kansas regulations (e.g., Kansas Department for Aging and Disability Services - KDADS), long-term care facilities must ensure residents receive care that supports their physical, mental, and psychosocial well-being. This includes proper documentation of diagnoses like COPD in care plans and adjusting activities to fit residents’ medical needs.
Understanding COPD is essential for Social Service Designees and Activities Directors in LTC facilities. By recognizing the symptoms and adjusting services accordingly, these professionals play a key role in improving residents’ comfort, emotional health, and quality of life.